http://www.jomi.com/article/1/Arthroscopic-Total-Shoulder-Resurfacing-with-Osteochondral-Allograft
Arthroscopic Total Shoulder Resurfacing with Osteochondral Allograft
Samuel Dubrow MD, Ruben Gobezie MD
1Cleveland Shoulder Service, University Hospitals of Cleveland, Case Medical Center
Text
Procedure Outline
Abstract
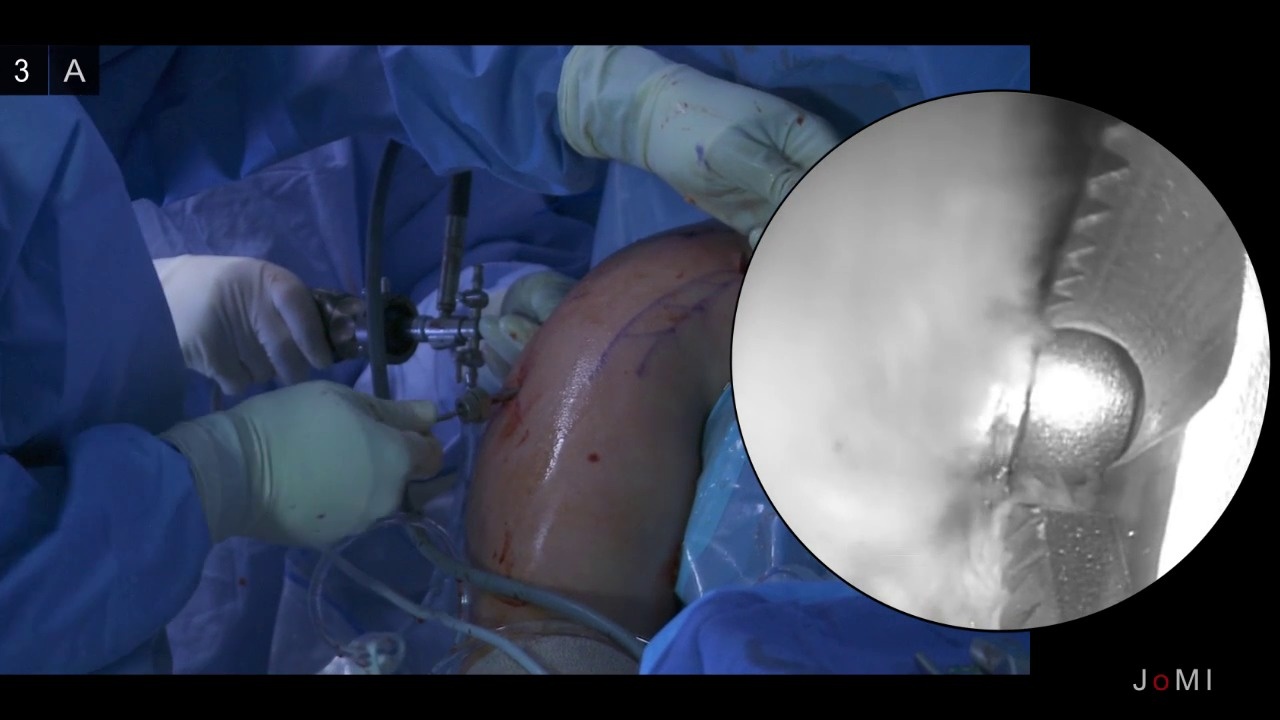
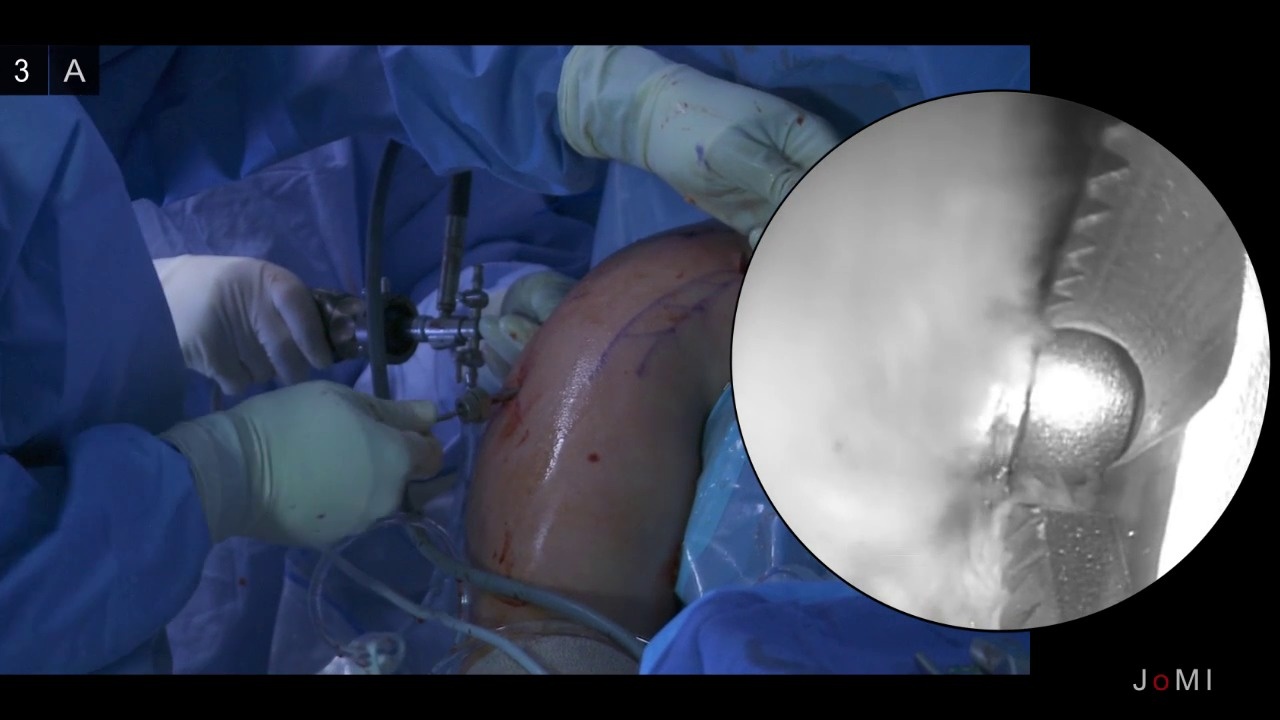
Limited treatment options exist for glenohumeral osteoarthritis in a young and active patient. To address the pain and limitation of significant osteoarthritis while avoiding a total shoulder arthroplasty (TSA), we have been using a minimally invasive technique to resurface both the glenoid and the humeral head using osteochondral allografts. After identifying the areas of most severe chondral damage during a diagnostic arthroscopy, a transhumeral tunnel is drilled using a transhumeral guidepin. Through this tunnel the allograft donor sites are prepared by retrograde reaming the humeral head and antegrade reaming the glenoid socket. Allograft constructs are sized and cut intra-operatively on a back table, inserted through the anterior portal and secured into the graft sites using chondral darts for the glenoid and a press fit for the humeral head.
Case Overview
Clinical presentation
This is a 53 year old right hand dominant male with right shoulder pain gradually worsening over the past three years. His pain is worse at night and with overhead motions and rates his pain as a 7-8 out of 10 at its worst. He has slightly decreased range of motion, most notably in internal rotation, and pain upon overhead lifting and forward flexion above 140 degrees. His pain interferes with his work as well as his quality of life, interfering with restful sleep.
He reports no loss of strength or numbness. Past history is significant for Type 2 Diabetes Mellitus and hypertension. He has had 2 corticosteroid injections which resulted in minimal pain relief. Treatment options were discussed with the patient, including observation, activity modification, repeat injections, occupational therapy and total shoulder replacement versus arthroscopic surgery to resurface the shoulder with allograft. Risks and benefits were discussed in detail with the patient and he requested the arthroscopic resurfacing procedure.
Physical Exam
On exam, he reported a pain severity of 7 out of 10 on forward flexion above 120 degrees. The shoulder is stable with a negative lift off test and there was no weakness appreciated to the rotator cuff upon static strength testing. There is mild loss of motion in all planes, with forward elevation to 160 degrees, external rotation to 40 degrees and internal rotation to L5. Passive range of motion is comparable to active range of motion with stiff end points in all planes. He has positive impingement signs, a positive speeds test and tenderness to palpation over the anterior aspect of his shoulder in the region of the proximal biceps tendon. He is neurovascularly intact distally to his right upper extremity with full range of motion to his right elbow, wrist and hand.
Imaging
Pre-operative AP and axillary radiographs reveal severe narrowing of the glenohumeral joint space and subchondral sclerosis Anterior-Posterior View
Anterior-Posterior View Axillary View
Axillary View
Natural history
Without intervention the expected natural clinical progression consists of worsening pain, increased severity of osteoarthritis, and further decreased shoulder range of motion.
Options for treatment
The options for treatment at this time include a repeat corticosteroid injection, physical therapy, NSAIDs, a total shoulder replacement, arthroscopic debridement and a resurfacing procedure with allograft.
Rationale for current procedure
This procedure avoids a total shoulder replacement in a relatively younger and active patient. Advantages include a shortened recovery period, no loss of strength, the subscapularis is kept intact and the relatively high risk of TSA implant failure in younger patients is avoided. As opposed to an open procedure, arthroscopy is less traumatic, has less risk of joint infection and allows for complete visualization of the shoulder joint.
Special considerations
The larger size of this patient's shoulder makes for a slightly challenging case. If the osteoarthritis was more extensive, the patient was not particularly active and over the age of 60 years, a total shoulder replacement would have been recommended.
Care needs to be taken when placing the transhumeral guide pin; the axillary nerve should be identified and kept clear of pin placement by blunt dissection down to the humeral cortex.
In a larger shoulder such as in this case, it is especially important to take care when inserting the allograft through the anterior arthroscopic portal not to lose control of the graft as retrieval would be potentially difficult.
Discussion
Glenohumeral arthritis remains a challenging issue to treat in the active young patient. This is due in most part to concerns regarding the longevity of a stable total shoulder prosthesis, specifically loosening, failure, and the eventual need for revision surgery. Young patients that wish to maintain a high level of activity may not be suited for traditional total shoulder replacement because of this concern of implant durability. Arthroscopic biologic total shoulder resurfacing with osteochondral allograft can be a promising alternative for the treatment of arthritis in a young individual. It also allows for bone conservation, so should the arthritis progress, a standard total shoulder replacement can readily be performed at a later date, if necessary.
This procedure has been performed by the senior author (RG) on 22 patients with a 2 year follow-up. Results have been promising with improvements in mean visual analog pain scores improving from 6 to 1. Range of motion in forward elevation has improved on average from 128 degrees to 137 degrees. The mean American Shoulder and Elbow Surgeons score in this patient population has also improved from 40 to 83. However, long term outcomes are not yet available.
Disclosures
Disclosures R.G is a consultant for and receives support from Arthrex, Naples FL
Statement of Consent
Informed consent was obtained from the patient and all staff present in the operating room to be filmed and are aware that portions of this video will be published and freely available online.
Equipment
Arthroscope - Stryker, Kalamazoo MI
Chondral Dart System - Arthrex, Naples FL
OATS system - Arthrex, Naples, FL
Special Acknowledgements
The authors would like to thank Ian Fein for his videography and the Operating Room staff for their help in making this video.
Citations
Boyd Jr, Allen D., et al. "Total shoulder arthroplasty versus hemiarthroplasty: indications for glenoid resurfacing." The Journal of arthroplasty 5.4 (1990): 329-336.
Wallace, Andrew L., et al. "Resurfacing of the Glenoid in Total Shoulder Arthroplasty. A Comparison, at a Mean of Five Years, of Prostheses Inserted with and without Cement*." The Journal of Bone & Joint Surgery 81.4 (1999): 510-8.
Burkhead Jr, W. Z., and Kirk S. Hutton. "Biologic resurfacing of the glenoid with hemiarthroplasty of the shoulder." Journal of Shoulder and Elbow Surgery 4.4 (1995): 263-270.
Gobezie, Reuben, et al. "All-arthroscopic biologic total shoulder resurfacing."Arthroscopy: The Journal of Arthroscopic & Related Surgery 27.11 (2011): 1588-1593.
Millett, Peter J., Gobezie, Reuben and Boykin, Robert E. "Shoulder osteoarthritis: diagnosis and management." Am Fam Physician 78.5 (2008): 605-611.
Dubrow, Samuel, Gobezie, Reuben. “Alternative options to traditional shoulder replacement: arthritis in the young patient.” Current Orthopaedic Practice 24.4 (2013): 370-375.
Dubrow, Samuel, Shishani, Yousef, Gobezie, Reuben. “Arthroscopic alternatives to total shoulder arthroplasty.” Seminars in Arthroplasty 24 (2013): 2-6
Arthroscopic Total Shoulder Resurfacing with Osteochondral Allograft
Samuel Dubrow MD, Ruben Gobezie MD
1Cleveland Shoulder Service, University Hospitals of Cleveland, Case Medical Center
Text
Procedure Outline
Abstract
Limited treatment options exist for glenohumeral osteoarthritis in a young and active patient. To address the pain and limitation of significant osteoarthritis while avoiding a total shoulder arthroplasty (TSA), we have been using a minimally invasive technique to resurface both the glenoid and the humeral head using osteochondral allografts. After identifying the areas of most severe chondral damage during a diagnostic arthroscopy, a transhumeral tunnel is drilled using a transhumeral guidepin. Through this tunnel the allograft donor sites are prepared by retrograde reaming the humeral head and antegrade reaming the glenoid socket. Allograft constructs are sized and cut intra-operatively on a back table, inserted through the anterior portal and secured into the graft sites using chondral darts for the glenoid and a press fit for the humeral head.
Case Overview
Clinical presentation
This is a 53 year old right hand dominant male with right shoulder pain gradually worsening over the past three years. His pain is worse at night and with overhead motions and rates his pain as a 7-8 out of 10 at its worst. He has slightly decreased range of motion, most notably in internal rotation, and pain upon overhead lifting and forward flexion above 140 degrees. His pain interferes with his work as well as his quality of life, interfering with restful sleep.
He reports no loss of strength or numbness. Past history is significant for Type 2 Diabetes Mellitus and hypertension. He has had 2 corticosteroid injections which resulted in minimal pain relief. Treatment options were discussed with the patient, including observation, activity modification, repeat injections, occupational therapy and total shoulder replacement versus arthroscopic surgery to resurface the shoulder with allograft. Risks and benefits were discussed in detail with the patient and he requested the arthroscopic resurfacing procedure.
Physical Exam
On exam, he reported a pain severity of 7 out of 10 on forward flexion above 120 degrees. The shoulder is stable with a negative lift off test and there was no weakness appreciated to the rotator cuff upon static strength testing. There is mild loss of motion in all planes, with forward elevation to 160 degrees, external rotation to 40 degrees and internal rotation to L5. Passive range of motion is comparable to active range of motion with stiff end points in all planes. He has positive impingement signs, a positive speeds test and tenderness to palpation over the anterior aspect of his shoulder in the region of the proximal biceps tendon. He is neurovascularly intact distally to his right upper extremity with full range of motion to his right elbow, wrist and hand.
Imaging
Pre-operative AP and axillary radiographs reveal severe narrowing of the glenohumeral joint space and subchondral sclerosis
 Anterior-Posterior View
Anterior-Posterior View Axillary View
Axillary ViewNatural history
Without intervention the expected natural clinical progression consists of worsening pain, increased severity of osteoarthritis, and further decreased shoulder range of motion.
Options for treatment
The options for treatment at this time include a repeat corticosteroid injection, physical therapy, NSAIDs, a total shoulder replacement, arthroscopic debridement and a resurfacing procedure with allograft.
Rationale for current procedure
This procedure avoids a total shoulder replacement in a relatively younger and active patient. Advantages include a shortened recovery period, no loss of strength, the subscapularis is kept intact and the relatively high risk of TSA implant failure in younger patients is avoided. As opposed to an open procedure, arthroscopy is less traumatic, has less risk of joint infection and allows for complete visualization of the shoulder joint.
Special considerations
The larger size of this patient's shoulder makes for a slightly challenging case. If the osteoarthritis was more extensive, the patient was not particularly active and over the age of 60 years, a total shoulder replacement would have been recommended.
Care needs to be taken when placing the transhumeral guide pin; the axillary nerve should be identified and kept clear of pin placement by blunt dissection down to the humeral cortex.
In a larger shoulder such as in this case, it is especially important to take care when inserting the allograft through the anterior arthroscopic portal not to lose control of the graft as retrieval would be potentially difficult.
Discussion
Glenohumeral arthritis remains a challenging issue to treat in the active young patient. This is due in most part to concerns regarding the longevity of a stable total shoulder prosthesis, specifically loosening, failure, and the eventual need for revision surgery. Young patients that wish to maintain a high level of activity may not be suited for traditional total shoulder replacement because of this concern of implant durability. Arthroscopic biologic total shoulder resurfacing with osteochondral allograft can be a promising alternative for the treatment of arthritis in a young individual. It also allows for bone conservation, so should the arthritis progress, a standard total shoulder replacement can readily be performed at a later date, if necessary.
This procedure has been performed by the senior author (RG) on 22 patients with a 2 year follow-up. Results have been promising with improvements in mean visual analog pain scores improving from 6 to 1. Range of motion in forward elevation has improved on average from 128 degrees to 137 degrees. The mean American Shoulder and Elbow Surgeons score in this patient population has also improved from 40 to 83. However, long term outcomes are not yet available.
Disclosures
Disclosures R.G is a consultant for and receives support from Arthrex, Naples FL
Statement of Consent
Informed consent was obtained from the patient and all staff present in the operating room to be filmed and are aware that portions of this video will be published and freely available online.
Equipment
Arthroscope - Stryker, Kalamazoo MI
Chondral Dart System - Arthrex, Naples FL
OATS system - Arthrex, Naples, FL
Special Acknowledgements
The authors would like to thank Ian Fein for his videography and the Operating Room staff for their help in making this video.
Citations
Boyd Jr, Allen D., et al. "Total shoulder arthroplasty versus hemiarthroplasty: indications for glenoid resurfacing." The Journal of arthroplasty 5.4 (1990): 329-336.
Wallace, Andrew L., et al. "Resurfacing of the Glenoid in Total Shoulder Arthroplasty. A Comparison, at a Mean of Five Years, of Prostheses Inserted with and without Cement*." The Journal of Bone & Joint Surgery 81.4 (1999): 510-8.
Burkhead Jr, W. Z., and Kirk S. Hutton. "Biologic resurfacing of the glenoid with hemiarthroplasty of the shoulder." Journal of Shoulder and Elbow Surgery 4.4 (1995): 263-270.
Gobezie, Reuben, et al. "All-arthroscopic biologic total shoulder resurfacing."Arthroscopy: The Journal of Arthroscopic & Related Surgery 27.11 (2011): 1588-1593.
Millett, Peter J., Gobezie, Reuben and Boykin, Robert E. "Shoulder osteoarthritis: diagnosis and management." Am Fam Physician 78.5 (2008): 605-611.
Dubrow, Samuel, Gobezie, Reuben. “Alternative options to traditional shoulder replacement: arthritis in the young patient.” Current Orthopaedic Practice 24.4 (2013): 370-375.
Dubrow, Samuel, Shishani, Yousef, Gobezie, Reuben. “Arthroscopic alternatives to total shoulder arthroplasty.” Seminars in Arthroplasty 24 (2013): 2-6

No hay comentarios:
Publicar un comentario