Dr Francisco Pérez Jiménez
viernes, 28 de marzo de 2014
jueves, 27 de marzo de 2014
Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Our current management of apparently aseptic shoul...
Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Our current management of apparently aseptic shoul...: We are often asked about our approach to the revision of stiff, painful or loose shoulder arthroplasties without obvious evidence of i...
Our current management of apparently aseptic shoulder arthroplasty failure
We are often asked about our approach to the revision of stiff, painful or loose shoulder arthroplasties without obvious evidence of infection (i.e. no fever, chills, swelling warmth, elevated sedimentation rate, elevated C reactive protein, elevated white blood cell count, draining sinus, etc). This approach is heavily influenced by two of our research studies as posted here and here.
Based on these studies we assume that a painful/stiff arthroplasty that has not responded to reasonable attempts at rehabilitation or a shoulder arthroplasty with component loosening and / or osteolysis is infected with either Propionibacterium or coagulase negative Staph until proven otherwise.
If the patient wishes to proceed with revision surgery after a detailed informed consent session, we plan a single stage exchange revision. At surgery, we harvest 5 non-fluid cultures (tissue or prosthesis explants) before prophylactic antibiotics are administered and send these specimens for Propionibacterium-specific cultures (aerobic, anaerobic and broth held for three weeks). If there is a high index of intraoperative suspicion (humeral membrane, osteolysis, male patient, component loosening, cloudy joint fluid) the patient is placed on a PICC line with Ceftriaxone+Vancomycin. We call this the 'red' protocol. If the index of suspicion is lower, we place the patient on oral Augmentin, the 'yellow' protocol. If the cultures become positive, our infectious disease service makes modification in the regimen (for example, if someone on the 'yellow' protocol grows out Propionibacterium the patient will be converted to IV antibiotics (as in the 'red' protocol)). If there is no growth at three weeks, we will usually stop antibiotics unless the surgical suspicion is high.
The surgical procedure usually involves removing all components (to exclude the possibility of biofilms perpetuating the infection) and reimplanting the humeral component with impaction grafting using Vancomycin soaked allograft.
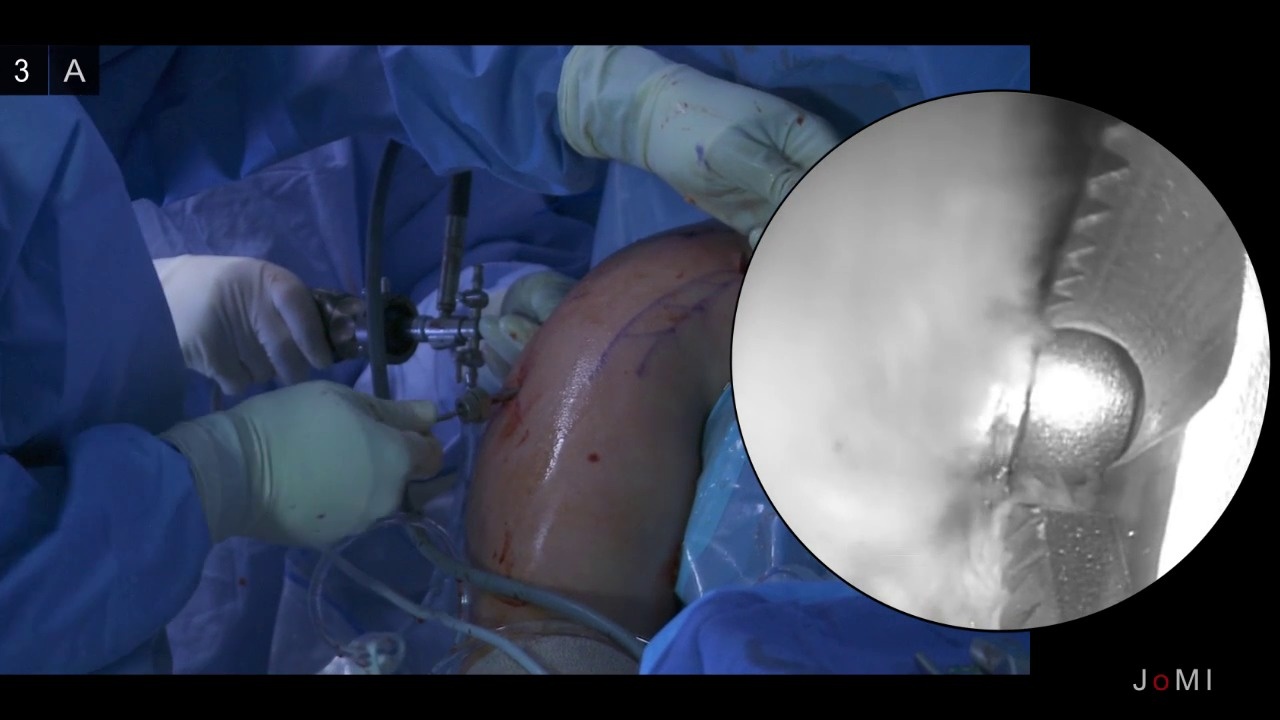
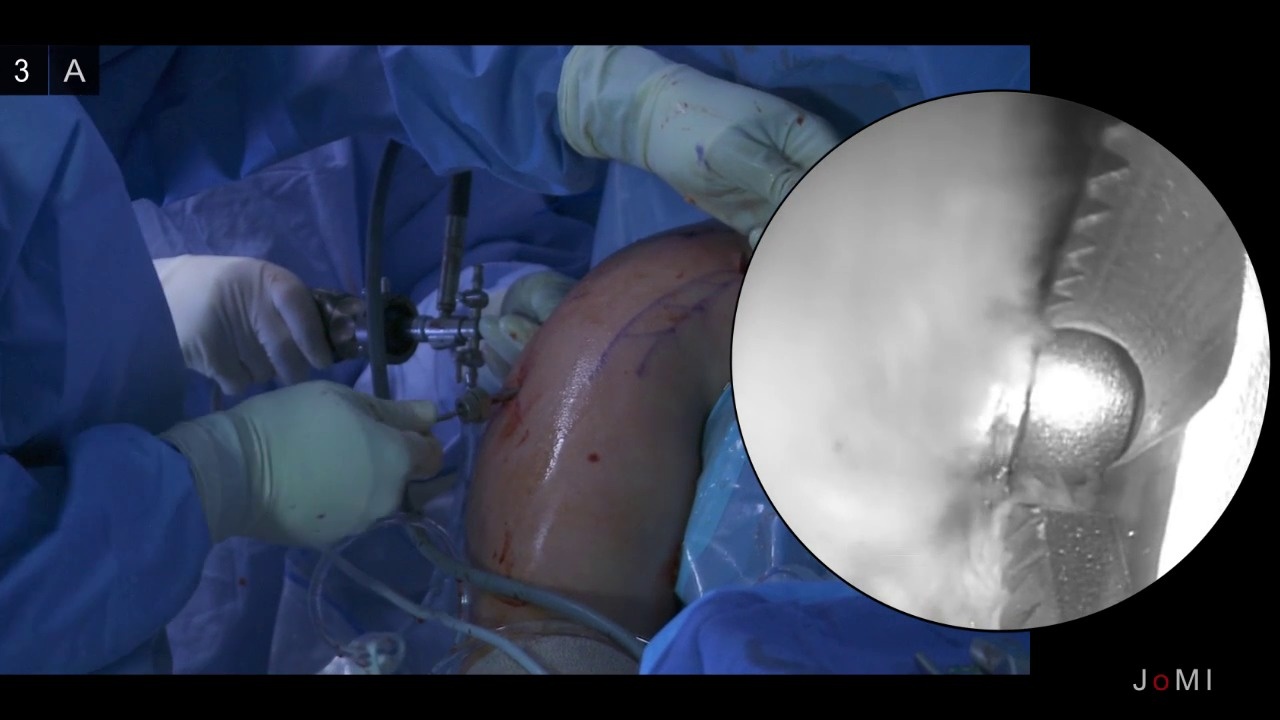
Here's a case from yesterday's OR schedule:
The surgical procedure usually involves removing all components (to exclude the possibility of biofilms perpetuating the infection) and reimplanting the humeral component with impaction grafting using Vancomycin soaked allograft.
Here's a case from yesterday's OR schedule:
This patient had a total shoulder arthroplasty done in 1997. Recently it became painful with loss of function. X-rays showed glenoid component loosening and osteolysis.
At surgery the shoulder showed extensive chronic inflammation, glenoid loosening and humeral osteolysis that was not evident on the preoprerative films.
The glenoid and humeral components were removed, the hypertrophic tissue was resected and a new humeral component was inserted with impaction allograft after vigorous irrigation with 3 liters of Vancomycin - Cephtriaxone solution.
The patient will have a PICC line placed today.
His rehabilitation is the same a that for a standard shoulder arthroplasty.
Today in clinic we saw a patient who had had this procedure a year ago and was pleased with the comfort and function of his shoulder.
Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Longer immobilization after rotator cuff repair ma...
Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Longer immobilization after rotator cuff repair ma...: Effect of Immobilization without Passive Exercise After Rotator Cuff Repair: Randomized Clinical Trial Comparing Four and Eight Weeks of Imm...
Thursday, March 27, 2014
Longer immobilization after rotator cuff repair may increase risk of stiffness
Effect of Immobilization without Passive Exercise After Rotator Cuff Repair: Randomized Clinical Trial Comparing Four and Eight Weeks of Immobilization
Surgeons continue to search for an optimal rehabilitation program after a rotator cuff repair.
may not really be 'immobilization" in that the patient must take the device off for bathing and changing clothes. It would be of interest to study the motion of shoulders that are thus 'immobilized'
Surgeons continue to search for an optimal rehabilitation program after a rotator cuff repair.
These authors assessed the effect of immobilization following rotator cuff repair in 100 patients who underwent arthroscopic single-row repair of a posterosuperior rotator cuff tear (mean, 2.3 cm in the coronal-oblique plane and 2.0 cm in the sagittal-oblique plane) who were prospectively randomized to be treated with immobilization for four or eight weeks using an abduction pillow.During the immobilization period, no passive or active range-of-motion exercise was allowed.
On MRI at 6 months after surgery, there were five full-thickness retears in the four-week group and four in the eight-week group. At the time of final follow-up, the two groups showed no differences in range of motion or clinical scores. However, the proportion showing stiffness was higher in the eight-week group (38% compared with 18%).
Patients with preoperative stiffness had approximately a 50% rate of postoperative stiffness regardless of the duration of immobilization.
Comment: Surgeons may use abduction pillows to take tension off the cuff repair or to protect it from loading from loading during activities. However, use of an abduction pillow
Patients with preoperative stiffness had approximately a 50% rate of postoperative stiffness regardless of the duration of immobilization.
Comment: Surgeons may use abduction pillows to take tension off the cuff repair or to protect it from loading from loading during activities. However, use of an abduction pillow
may not really be 'immobilization" in that the patient must take the device off for bathing and changing clothes. It would be of interest to study the motion of shoulders that are thus 'immobilized'
Use of such a device represents an inconvenience for the patient in terms of their ability to get around and may actually result in increased movement of the arm as the patient moves from the standing to the lying position. It would seem that the maximal challenge to repair integrity would come during the position changes when the pillow is temporarily moved or when the pillow shifts on the body.
In any event, it is nice to see a randomized trial and to have attention called to the issue of stiffness after cuff repair.
Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Rotator cuff repair, can the healing be enhanced?
Shoulder Arthritis / Rotator Cuff Tears: causes of shoulder pain: Rotator cuff repair, can the healing be enhanced?: Re-establishing the complex anatomy of the tendon attachment to bone is a major challenge in orthopedics. The authors of Augmentati...
They looked at a number of different approaches. These are listed below along with their conclusions.
Osteoinductive Growth Factors
Transforming growth factor, bone morphogenetic protein, fibroblast growth factor, and granulocyte colony-stimulating factor have shown some positive effects on the repair and healing of tendon and bone tissues in animal model studies.
Platelet-Rich Plasma
Although basic-science studies suggest positive effects on tendon-to-bone healing, clinical evidence from controlled human trials involving rotator cuff tendons does not show any superiority of platelet rich plasma augmented repairs over conventional methods.
Gene Therapy
Viral or nonviral vehicles can be used genetically modify cells to express growth factor at the tendon-bone insertion site. Before gene transfer can be tried as a therapeutic method to improve tendon-to-bone healing in humans, questions regarding safety and regulatory issues need to be answered.
Enveloping The Grafts With Periosteum
While enveloping the grafts with periosteum appears to be a promising approach, clinical evidence supporting its use in humans to augment tendon-to-bone healing is lacking.
Osteoconductive Materials
Calcium or magnesium-based osteoconductive materials are readily available and relatively inexpensive compared with other biological treatment modalities. Further research is required to prove them as biocompatible and effective treatment alternatives to reconstruct the tendon-to-bone interface in humans.
Cell-Based Therapies
The knowledge about the conditions that are required to choose a certain type of stem cell, optimum cell amount, and delivery vehicles, is limited. Serious concerns exist regarding their potential for differentiation into undesirable lineages, which could result in tumor-like growth.
Biodegradable Scaffolds And Biomimetic Patches
Biocompatible and biodegradable scaffolds with porous ultrastructure permit invasion and easy attachment of cells, while creating an environment suitable for cell proliferation and differentiation as demonstrated in models. The success of these approaches will require a thorough understanding of the structure-function relationship at the native insertion site, as well as the elucidation of the mechanisms governing interface regeneration.
Low-Intensity Pulsed Ultrasound
Low-intensity pulsed ultrasound may promote osteoblast and fibroblast proliferation, which may contributes to improved collagen formation and bone remodeling.
Extracorporeal Shockwave Treatment
Extracorporeal shockwave treatment can affect bone by exertion of direct pressure or by causing cavitation. These factors may create an environment with a better blood supply and increased bone and collagen formation, which may create a stronger tendon-to-bone interface.
Effects Of Various Loading Methods And Immobilization On Interface Healing
On the basis of animal models, neither strict immobilization nor immediate initiation of rehabilitation and loading appear to be beneficial after surgical repair, but rather a balance between the modalities is needed to optimize the healing enthesis and obtain a stronger interface.
Coated Sutures And Interference Screws
As with other growth factor delivery vehicles, challenges remain, including timing, dosages, degree of elution, sustainability of the release, effects of coating on fixative materials, and safety.
Delayed Interface Healing
Research is attempting to identify molecules and/or conditions that may delay the healing of the tendon-bone interface. Evidence from animal model studies has also shown that conditions that negatively impact bone formation and fracture-healing, such as uncontrolled diabetes mellitus, nicotine, and nonsteroidal anti-inflammatory drugs, also negatively affect tendon-to-bone healing.
Thursday, March 27, 2014
Rotator cuff repair, can the healing be enhanced?
The authors of Augmentation of Tendon-to-Bone Healing review some of the methods currently under investigation for increasing the quality of this complex healing challenge.
Osteoinductive Growth Factors
Transforming growth factor, bone morphogenetic protein, fibroblast growth factor, and granulocyte colony-stimulating factor have shown some positive effects on the repair and healing of tendon and bone tissues in animal model studies.
Platelet-Rich Plasma
Although basic-science studies suggest positive effects on tendon-to-bone healing, clinical evidence from controlled human trials involving rotator cuff tendons does not show any superiority of platelet rich plasma augmented repairs over conventional methods.
Gene Therapy
Viral or nonviral vehicles can be used genetically modify cells to express growth factor at the tendon-bone insertion site. Before gene transfer can be tried as a therapeutic method to improve tendon-to-bone healing in humans, questions regarding safety and regulatory issues need to be answered.
Enveloping The Grafts With Periosteum
While enveloping the grafts with periosteum appears to be a promising approach, clinical evidence supporting its use in humans to augment tendon-to-bone healing is lacking.
Osteoconductive Materials
Calcium or magnesium-based osteoconductive materials are readily available and relatively inexpensive compared with other biological treatment modalities. Further research is required to prove them as biocompatible and effective treatment alternatives to reconstruct the tendon-to-bone interface in humans.
Cell-Based Therapies
The knowledge about the conditions that are required to choose a certain type of stem cell, optimum cell amount, and delivery vehicles, is limited. Serious concerns exist regarding their potential for differentiation into undesirable lineages, which could result in tumor-like growth.
Biodegradable Scaffolds And Biomimetic Patches
Biocompatible and biodegradable scaffolds with porous ultrastructure permit invasion and easy attachment of cells, while creating an environment suitable for cell proliferation and differentiation as demonstrated in models. The success of these approaches will require a thorough understanding of the structure-function relationship at the native insertion site, as well as the elucidation of the mechanisms governing interface regeneration.
Low-Intensity Pulsed Ultrasound
Low-intensity pulsed ultrasound may promote osteoblast and fibroblast proliferation, which may contributes to improved collagen formation and bone remodeling.
Extracorporeal shockwave treatment can affect bone by exertion of direct pressure or by causing cavitation. These factors may create an environment with a better blood supply and increased bone and collagen formation, which may create a stronger tendon-to-bone interface.
Effects Of Various Loading Methods And Immobilization On Interface Healing
On the basis of animal models, neither strict immobilization nor immediate initiation of rehabilitation and loading appear to be beneficial after surgical repair, but rather a balance between the modalities is needed to optimize the healing enthesis and obtain a stronger interface.
Coated Sutures And Interference Screws
As with other growth factor delivery vehicles, challenges remain, including timing, dosages, degree of elution, sustainability of the release, effects of coating on fixative materials, and safety.
Delayed Interface Healing
Research is attempting to identify molecules and/or conditions that may delay the healing of the tendon-bone interface. Evidence from animal model studies has also shown that conditions that negatively impact bone formation and fracture-healing, such as uncontrolled diabetes mellitus, nicotine, and nonsteroidal anti-inflammatory drugs, also negatively affect tendon-to-bone healing.
Conclusion:
Knowledge about the complexity of tendon-to-bone healing is still limited and mainly based on animal studies. Rigorous clinical trials must be conducted to determine the value - benefit/(cost+risk) - of these approaches.
As we've pointed out in prior posts, atraumatic failure of the rotator cuff insertion is adegenerative process. Even if we could artificially manipulate the environment at the site of surgical reattachment, we not be able to "un-degenerate" the tendon or to prevent repeat failure after surgery.
As we've pointed out in prior posts, atraumatic failure of the rotator cuff insertion is adegenerative process. Even if we could artificially manipulate the environment at the site of surgical reattachment, we not be able to "un-degenerate" the tendon or to prevent repeat failure after surgery.
viernes, 21 de marzo de 2014
Shoulder Arthroscopy Anatomy
Shoulder Arthroscopy Anatomy
Subido el 19/09/2008
10 Point shoulder arthroscopy. Key areas to look for common pathology.
from shoulderdoc.co.uk
from shoulderdoc.co.uk
jueves, 20 de marzo de 2014
viernes, 14 de marzo de 2014
MRI frente ecografía para evaluar Anomalías meniscales en las rodillas agudas / MRI versus Ultrasonography to Assess Meniscal Abnormalities in Acute Knees
http://www.ncbi.nlm.nih.gov/m/pubmed/24474166/
Resumen:
Mientras que la resonancia magnética ( RM) a menudo se considera el " patrón oro " modalidad de imagen de diagnóstico para la detección de anomalías de menisco , se asocia con un mal diagnóstico en tan alta como 47 % de los casos , es costoso , y no está fácilmente disponible para un gran número de los pacientes . Examen ecográfico de la rodilla ha sido informado de que una herramienta de diagnóstico eficaz para este propósito con el potencial para superar muchas de las deficiencias de la RM . El propósito de este estudio es determinar la utilidad clínica de la ecografía para el diagnóstico de la patología meniscal en pacientes con dolor de rodilla agudo y comparar su precisión diagnóstica de la RM en un entorno clínico. Con la aprobación de la Junta de Revisión Institucional , los pacientes (n = 71 ) con dolor de rodilla agudo se realizó un estudio prospectivo con el consentimiento informado . Preoperatorio RM ( 1,5 T) se realizó en cada rodilla afectada utilizando equipos y protocolos estándar del hospital y leídos por radiólogos profesores capacitados en RM musculoesquelética . Evaluaciones ecográficas de cada rodilla afectada fueron realizados por uno de los dos miembros de la facultad formados en ecografía musculoesquelética usando un transductor MHz lineal de 10 a 14. Evaluación artroscópica de las rodillas afectadas fue realizada por uno de los tres cirujanos ortopédicos de la facultad para evaluar y registrar toda la patología articular, que sirvió como patrón de referencia para determinar la presencia , tipo y gravedad de la patología meniscal . Todos los evaluadores para cada modalidad diagnóstica fueron cegados a todos los demás datos . Los datos fueron recolectados y comparados por un investigador independiente para determinar la sensibilidad (Sn ) , especificidad (E ) , valor predictivo positivo ( VPP) y valor predictivo negativo (VPN ) , la tasa de clasificación correcta (CCR ) , los cocientes de probabilidad ( LR [ +] y LR [ - ] ) , y la odds ratio . Evaluación ecográfica preoperatoria de la patología meniscal se asoció con Sn = 91.2 %, E = 84,2 %, VPP = 94,5 %, VPN = 76,2 % , CCR = 89,5 % , LR ( +) = 5,78 y LR ( -) = 0,10 . La evaluación preoperatoria de la patología meniscal MRI se asoció con Sn = 91.7 %, E = 66,7 %, VPP = 84,6 %, VPN = 80,0 % , CCR = 81,1 % , LR ( +) = 2,75 y LR ( -) = 0,13. La ecografía fue dos veces más propensos que la resonancia magnética para determinar correctamente la presencia o ausencia de patología meniscal mediante artroscopia visto en este estudio. La ecografía es una herramienta útil para el diagnóstico de la patología meniscal con ventajas potenciales sobre la resonancia magnética. Sobre la base de estos datos y el equipo portátil disponible , la ecografía se podría considerar para su uso como una modalidad de diagnóstico de punto de lesión para las lesiones de menisco .
Thieme Medical Publishers 333 Seventh Avenue, Nueva York, NY 10001, EE.UU. .
PMID 24474166 [PubMed - según lo provisto por el editor]
Texto completo : Georg Thieme Verlag Stuttgart , Nueva York
Abstract
While magnetic resonance imaging (MRI) is often considered the "gold standard" diagnostic imaging modality for detection of meniscal abnormalities, it is associated with misdiagnosis in as high as 47% of cases, is costly, and is not readily available to a large number of patients. Ultrasonographic examination of the knee has been reported to be an effective diagnostic tool for this purpose with the potential to overcome many of the shortcomings of MRI. The purpose of this study is to determine the clinical usefulness of ultrasonography for diagnosis of meniscal pathology in patients with acute knee pain and compare its diagnostic accuracy to MRI in a clinical setting. With Institutional Review Board approval, patients (n = 71) with acute knee pain were prospectively enrolled with informed consent. Preoperative MRI (1.5 T) was performed on each affected knee using the hospital's standard equipment and protocols and read by faculty radiologists trained in musculoskeletal MRI. Ultrasonographic assessments of each affected knee were performed by one of two faculty members trained in musculoskeletal ultrasonography using a 10 to 14 MHz linear transducer. Arthroscopic evaluation of affected knees was performed by one of three faculty orthopedic surgeons to assess and record all joint pathology, which served as the reference standard for determining presence, type, and severity of meniscal pathology. All evaluators for each diagnostic modality were blinded to all other data. Data were collected and compared by a separate investigator to determine sensitivity (Sn), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), correct classification rate (CCR), likelihood ratios (LR[+] and LR[-]), and odds ratios. Preoperative ultrasonographic assessment of meniscal pathology was associated with Sn = 91.2%, Sp = 84.2%, PPV = 94.5%, NPV = 76.2%, CCR = 89.5%, LR(+) = 5.78, and LR(-) = 0.10. Preoperative MRI assessment of meniscal pathology was associated with Sn = 91.7%, Sp = 66.7%, PPV = 84.6%, NPV = 80.0%, CCR = 81.1%, LR(+) = 2.75, and LR(-) = 0.13. Ultrasonography was two times more likely than MRI to correctly determine presence or absence of meniscal pathology seen arthroscopically in this study. Ultrasonography is a useful tool for diagnosis of meniscal pathology with potential advantages over MRI. Based on these data and available portable equipment, ultrasonography could be considered for use as a point-of-injury diagnostic modality for meniscal injuries.
Thieme Medical Publishers 333 Seventh Avenue, New York, NY 10001, USA.PMID
24474166 [PubMed - as supplied by publisher]
Full text: Georg Thieme Verlag Stuttgart, New York
Tibial fixation in anterior cruciate ligament reconstruction: a prospective randomized study comparing metal interference screw and staples with a centrally placed polyethylene screw and sheath
Fuente original de esta cita:
http://www.ncbi.nlm.nih.gov/pubmed/21622815
http://www.ncbi.nlm.nih.gov/pubmed/21622815
Am J Sports Med. 2011 Sep;39(9):1858-64. doi: 10.1177/0363546511406234. Epub 2011 May 27.
Tibial fixation in anterior cruciate ligament reconstruction: a prospective randomized study comparing metal interference screw and staples with a centrally placed polyethylene screw and sheath.
Abstract
BACKGROUND:
The use of hamstring tendons for anterior cruciate ligament reconstruction has increased in popularity over recent years. However, concerns with the stability of graft fixation on the tibial side remain. Centrally placed interference screw/sheath implants have demonstrated promising results in biomechanical studies.
HYPOTHESIS:
Centrally placed, polyethylene screw and sheath implants will provide clinically equivalent fixation to the standard metal interference screw and supplemental staple fixation. Study Design: Randomized controlled trial; Level of evidence, 1.
METHODS:
A total of 113 consecutive patients undergoing isolated, unilateral, primary anterior cruciate ligament reconstruction with hamstring autografts were randomized to tibial fixation with metal interference screw and staples (RCI) or with a centrally placed polyethylene screw and sheath implant (INTRAFIX). Prospective assessment of subjective outcomes was performed using Lysholm, Mohtadi, and International Knee Documentation Committee (IKDC) scores.
RESULTS:
At minimum 2-year follow-up, there were no significant differences between the 2 groups in terms of instrumented stability testing (KT-1000 arthrometer) or subjective assessment of knee outcomes (IKDC, Lysholm, Mohtadi). Both fixation methods demonstrated a significant, but not different, increase in outcomes scores from preoperative to postoperative evaluation. There were 7 failures (5 INTRAFIX, 2 RCI) caused by reinjury, but no statistically significant differences were observed between the 2 fixation methods.
CONCLUSION:
The centrally placed polyethylene screw and sheath provided equivalent clinical outcomes at minimum 2-year follow-up to standard tibial fixation with metal interference screw and staples.
- PMID:
- 21622815
- [PubMed - indexed for MEDLINE]
domingo, 9 de marzo de 2014
Meniscocidio: reparar el menisco o asesinarlo.
http://blog.clinicacemtro.com/especialidades/traumatologia-ortopedia-y-medicina-del-deporte/meniscocidio-reparar-el-menisco-o-asesinarlo/
Meniscocidio: reparar el menisco o asesinarlo.
Desde hace años sabemos que la extirpación del menisco supone una agresión severa para la rodilla, que altera la congruencia articular, expone el cartílago al roce y facilita la aparición de artrosis. Un reciente meta-análisis (el tipo de estudio científico de mayor fiabilidad, que repasa todos los estudios que hay sobre un mismo tema y hace un cálculo global de los resultados) concluye que los pacientes operados de desgarro de menisco mediante sutura o reparación meniscal tienen mejores resultados que los que se someten a meniscectomia total o parcial.
La meniscectomía sigue teniendo sus indicaciones, y hay pacientes y circunstancias en que es la mejor opción quirúrgica; sin embargo el objetivo del traumatólogo será, habitualmente, salvar los meniscos. El problema en que la cirugía de reparación, la sutura, es más difícil técnicamente que la meniscectomía, sobre todo cuando se hacer por artroscopia, lo que lleva que muchas veces se opte por la última opción, por ser más sencilla o porque necesita menor maestría en la técnica.
Ha habido una gran campaña para concienciar a la comunidad de traumatólogos de lo importante que es intentar salvar los meniscos (el Dr. Guillén acuñó el término “meniscocidio”, para dar relevancia a este acto que mutila la articulación); y los especialistas están desarrollando técnicas y aparatos que hacen que la reparación meniscal sea cada vez más sencilla y pueda realizarse en todo tipo de lesiones. Sin embargo, otro estudio reciente, en EEUU, apunta que en los últimos años el número de lesiones que se tratan mediante meniscectomía o mediante sutura meniscal no ha variado sustancialmente. Aunque estos datos no son extrapolables a España, si que dan una preocupante idea de lo que puede estar ocurriendo: que los cirujanos siguen optando por la alternativa tradicional, más sencilla. Que bien por desconocimiento técnico o por falta de experiencia, se siguen cometiendo meniscocidios.
sábado, 8 de marzo de 2014
viernes, 7 de marzo de 2014
Arthroscopic Total Shoulder Resurfacing with Osteochondral Allograft
http://www.jomi.com/article/1/Arthroscopic-Total-Shoulder-Resurfacing-with-Osteochondral-Allograft
Arthroscopic Total Shoulder Resurfacing with Osteochondral Allograft
Samuel Dubrow MD, Ruben Gobezie MD
1Cleveland Shoulder Service, University Hospitals of Cleveland, Case Medical Center
Text
Procedure Outline
Abstract
Limited treatment options exist for glenohumeral osteoarthritis in a young and active patient. To address the pain and limitation of significant osteoarthritis while avoiding a total shoulder arthroplasty (TSA), we have been using a minimally invasive technique to resurface both the glenoid and the humeral head using osteochondral allografts. After identifying the areas of most severe chondral damage during a diagnostic arthroscopy, a transhumeral tunnel is drilled using a transhumeral guidepin. Through this tunnel the allograft donor sites are prepared by retrograde reaming the humeral head and antegrade reaming the glenoid socket. Allograft constructs are sized and cut intra-operatively on a back table, inserted through the anterior portal and secured into the graft sites using chondral darts for the glenoid and a press fit for the humeral head.
Case Overview
Clinical presentation
This is a 53 year old right hand dominant male with right shoulder pain gradually worsening over the past three years. His pain is worse at night and with overhead motions and rates his pain as a 7-8 out of 10 at its worst. He has slightly decreased range of motion, most notably in internal rotation, and pain upon overhead lifting and forward flexion above 140 degrees. His pain interferes with his work as well as his quality of life, interfering with restful sleep.
He reports no loss of strength or numbness. Past history is significant for Type 2 Diabetes Mellitus and hypertension. He has had 2 corticosteroid injections which resulted in minimal pain relief. Treatment options were discussed with the patient, including observation, activity modification, repeat injections, occupational therapy and total shoulder replacement versus arthroscopic surgery to resurface the shoulder with allograft. Risks and benefits were discussed in detail with the patient and he requested the arthroscopic resurfacing procedure.
Physical Exam
On exam, he reported a pain severity of 7 out of 10 on forward flexion above 120 degrees. The shoulder is stable with a negative lift off test and there was no weakness appreciated to the rotator cuff upon static strength testing. There is mild loss of motion in all planes, with forward elevation to 160 degrees, external rotation to 40 degrees and internal rotation to L5. Passive range of motion is comparable to active range of motion with stiff end points in all planes. He has positive impingement signs, a positive speeds test and tenderness to palpation over the anterior aspect of his shoulder in the region of the proximal biceps tendon. He is neurovascularly intact distally to his right upper extremity with full range of motion to his right elbow, wrist and hand.
Imaging
Pre-operative AP and axillary radiographs reveal severe narrowing of the glenohumeral joint space and subchondral sclerosis Anterior-Posterior View
Anterior-Posterior View Axillary View
Axillary View
Natural history
Without intervention the expected natural clinical progression consists of worsening pain, increased severity of osteoarthritis, and further decreased shoulder range of motion.
Options for treatment
The options for treatment at this time include a repeat corticosteroid injection, physical therapy, NSAIDs, a total shoulder replacement, arthroscopic debridement and a resurfacing procedure with allograft.
Rationale for current procedure
This procedure avoids a total shoulder replacement in a relatively younger and active patient. Advantages include a shortened recovery period, no loss of strength, the subscapularis is kept intact and the relatively high risk of TSA implant failure in younger patients is avoided. As opposed to an open procedure, arthroscopy is less traumatic, has less risk of joint infection and allows for complete visualization of the shoulder joint.
Special considerations
The larger size of this patient's shoulder makes for a slightly challenging case. If the osteoarthritis was more extensive, the patient was not particularly active and over the age of 60 years, a total shoulder replacement would have been recommended.
Care needs to be taken when placing the transhumeral guide pin; the axillary nerve should be identified and kept clear of pin placement by blunt dissection down to the humeral cortex.
In a larger shoulder such as in this case, it is especially important to take care when inserting the allograft through the anterior arthroscopic portal not to lose control of the graft as retrieval would be potentially difficult.
Discussion
Glenohumeral arthritis remains a challenging issue to treat in the active young patient. This is due in most part to concerns regarding the longevity of a stable total shoulder prosthesis, specifically loosening, failure, and the eventual need for revision surgery. Young patients that wish to maintain a high level of activity may not be suited for traditional total shoulder replacement because of this concern of implant durability. Arthroscopic biologic total shoulder resurfacing with osteochondral allograft can be a promising alternative for the treatment of arthritis in a young individual. It also allows for bone conservation, so should the arthritis progress, a standard total shoulder replacement can readily be performed at a later date, if necessary.
This procedure has been performed by the senior author (RG) on 22 patients with a 2 year follow-up. Results have been promising with improvements in mean visual analog pain scores improving from 6 to 1. Range of motion in forward elevation has improved on average from 128 degrees to 137 degrees. The mean American Shoulder and Elbow Surgeons score in this patient population has also improved from 40 to 83. However, long term outcomes are not yet available.
Disclosures
Disclosures R.G is a consultant for and receives support from Arthrex, Naples FL
Statement of Consent
Informed consent was obtained from the patient and all staff present in the operating room to be filmed and are aware that portions of this video will be published and freely available online.
Equipment
Arthroscope - Stryker, Kalamazoo MI
Chondral Dart System - Arthrex, Naples FL
OATS system - Arthrex, Naples, FL
Special Acknowledgements
The authors would like to thank Ian Fein for his videography and the Operating Room staff for their help in making this video.
Citations
Boyd Jr, Allen D., et al. "Total shoulder arthroplasty versus hemiarthroplasty: indications for glenoid resurfacing." The Journal of arthroplasty 5.4 (1990): 329-336.
Wallace, Andrew L., et al. "Resurfacing of the Glenoid in Total Shoulder Arthroplasty. A Comparison, at a Mean of Five Years, of Prostheses Inserted with and without Cement*." The Journal of Bone & Joint Surgery 81.4 (1999): 510-8.
Burkhead Jr, W. Z., and Kirk S. Hutton. "Biologic resurfacing of the glenoid with hemiarthroplasty of the shoulder." Journal of Shoulder and Elbow Surgery 4.4 (1995): 263-270.
Gobezie, Reuben, et al. "All-arthroscopic biologic total shoulder resurfacing."Arthroscopy: The Journal of Arthroscopic & Related Surgery 27.11 (2011): 1588-1593.
Millett, Peter J., Gobezie, Reuben and Boykin, Robert E. "Shoulder osteoarthritis: diagnosis and management." Am Fam Physician 78.5 (2008): 605-611.
Dubrow, Samuel, Gobezie, Reuben. “Alternative options to traditional shoulder replacement: arthritis in the young patient.” Current Orthopaedic Practice 24.4 (2013): 370-375.
Dubrow, Samuel, Shishani, Yousef, Gobezie, Reuben. “Arthroscopic alternatives to total shoulder arthroplasty.” Seminars in Arthroplasty 24 (2013): 2-6
Arthroscopic Total Shoulder Resurfacing with Osteochondral Allograft
Samuel Dubrow MD, Ruben Gobezie MD
1Cleveland Shoulder Service, University Hospitals of Cleveland, Case Medical Center
Text
Procedure Outline
Abstract
Limited treatment options exist for glenohumeral osteoarthritis in a young and active patient. To address the pain and limitation of significant osteoarthritis while avoiding a total shoulder arthroplasty (TSA), we have been using a minimally invasive technique to resurface both the glenoid and the humeral head using osteochondral allografts. After identifying the areas of most severe chondral damage during a diagnostic arthroscopy, a transhumeral tunnel is drilled using a transhumeral guidepin. Through this tunnel the allograft donor sites are prepared by retrograde reaming the humeral head and antegrade reaming the glenoid socket. Allograft constructs are sized and cut intra-operatively on a back table, inserted through the anterior portal and secured into the graft sites using chondral darts for the glenoid and a press fit for the humeral head.
Case Overview
Clinical presentation
This is a 53 year old right hand dominant male with right shoulder pain gradually worsening over the past three years. His pain is worse at night and with overhead motions and rates his pain as a 7-8 out of 10 at its worst. He has slightly decreased range of motion, most notably in internal rotation, and pain upon overhead lifting and forward flexion above 140 degrees. His pain interferes with his work as well as his quality of life, interfering with restful sleep.
He reports no loss of strength or numbness. Past history is significant for Type 2 Diabetes Mellitus and hypertension. He has had 2 corticosteroid injections which resulted in minimal pain relief. Treatment options were discussed with the patient, including observation, activity modification, repeat injections, occupational therapy and total shoulder replacement versus arthroscopic surgery to resurface the shoulder with allograft. Risks and benefits were discussed in detail with the patient and he requested the arthroscopic resurfacing procedure.
Physical Exam
On exam, he reported a pain severity of 7 out of 10 on forward flexion above 120 degrees. The shoulder is stable with a negative lift off test and there was no weakness appreciated to the rotator cuff upon static strength testing. There is mild loss of motion in all planes, with forward elevation to 160 degrees, external rotation to 40 degrees and internal rotation to L5. Passive range of motion is comparable to active range of motion with stiff end points in all planes. He has positive impingement signs, a positive speeds test and tenderness to palpation over the anterior aspect of his shoulder in the region of the proximal biceps tendon. He is neurovascularly intact distally to his right upper extremity with full range of motion to his right elbow, wrist and hand.
Imaging
Pre-operative AP and axillary radiographs reveal severe narrowing of the glenohumeral joint space and subchondral sclerosis
 Anterior-Posterior View
Anterior-Posterior View Axillary View
Axillary ViewNatural history
Without intervention the expected natural clinical progression consists of worsening pain, increased severity of osteoarthritis, and further decreased shoulder range of motion.
Options for treatment
The options for treatment at this time include a repeat corticosteroid injection, physical therapy, NSAIDs, a total shoulder replacement, arthroscopic debridement and a resurfacing procedure with allograft.
Rationale for current procedure
This procedure avoids a total shoulder replacement in a relatively younger and active patient. Advantages include a shortened recovery period, no loss of strength, the subscapularis is kept intact and the relatively high risk of TSA implant failure in younger patients is avoided. As opposed to an open procedure, arthroscopy is less traumatic, has less risk of joint infection and allows for complete visualization of the shoulder joint.
Special considerations
The larger size of this patient's shoulder makes for a slightly challenging case. If the osteoarthritis was more extensive, the patient was not particularly active and over the age of 60 years, a total shoulder replacement would have been recommended.
Care needs to be taken when placing the transhumeral guide pin; the axillary nerve should be identified and kept clear of pin placement by blunt dissection down to the humeral cortex.
In a larger shoulder such as in this case, it is especially important to take care when inserting the allograft through the anterior arthroscopic portal not to lose control of the graft as retrieval would be potentially difficult.
Discussion
Glenohumeral arthritis remains a challenging issue to treat in the active young patient. This is due in most part to concerns regarding the longevity of a stable total shoulder prosthesis, specifically loosening, failure, and the eventual need for revision surgery. Young patients that wish to maintain a high level of activity may not be suited for traditional total shoulder replacement because of this concern of implant durability. Arthroscopic biologic total shoulder resurfacing with osteochondral allograft can be a promising alternative for the treatment of arthritis in a young individual. It also allows for bone conservation, so should the arthritis progress, a standard total shoulder replacement can readily be performed at a later date, if necessary.
This procedure has been performed by the senior author (RG) on 22 patients with a 2 year follow-up. Results have been promising with improvements in mean visual analog pain scores improving from 6 to 1. Range of motion in forward elevation has improved on average from 128 degrees to 137 degrees. The mean American Shoulder and Elbow Surgeons score in this patient population has also improved from 40 to 83. However, long term outcomes are not yet available.
Disclosures
Disclosures R.G is a consultant for and receives support from Arthrex, Naples FL
Statement of Consent
Informed consent was obtained from the patient and all staff present in the operating room to be filmed and are aware that portions of this video will be published and freely available online.
Equipment
Arthroscope - Stryker, Kalamazoo MI
Chondral Dart System - Arthrex, Naples FL
OATS system - Arthrex, Naples, FL
Special Acknowledgements
The authors would like to thank Ian Fein for his videography and the Operating Room staff for their help in making this video.
Citations
Boyd Jr, Allen D., et al. "Total shoulder arthroplasty versus hemiarthroplasty: indications for glenoid resurfacing." The Journal of arthroplasty 5.4 (1990): 329-336.
Wallace, Andrew L., et al. "Resurfacing of the Glenoid in Total Shoulder Arthroplasty. A Comparison, at a Mean of Five Years, of Prostheses Inserted with and without Cement*." The Journal of Bone & Joint Surgery 81.4 (1999): 510-8.
Burkhead Jr, W. Z., and Kirk S. Hutton. "Biologic resurfacing of the glenoid with hemiarthroplasty of the shoulder." Journal of Shoulder and Elbow Surgery 4.4 (1995): 263-270.
Gobezie, Reuben, et al. "All-arthroscopic biologic total shoulder resurfacing."Arthroscopy: The Journal of Arthroscopic & Related Surgery 27.11 (2011): 1588-1593.
Millett, Peter J., Gobezie, Reuben and Boykin, Robert E. "Shoulder osteoarthritis: diagnosis and management." Am Fam Physician 78.5 (2008): 605-611.
Dubrow, Samuel, Gobezie, Reuben. “Alternative options to traditional shoulder replacement: arthritis in the young patient.” Current Orthopaedic Practice 24.4 (2013): 370-375.
Dubrow, Samuel, Shishani, Yousef, Gobezie, Reuben. “Arthroscopic alternatives to total shoulder arthroplasty.” Seminars in Arthroplasty 24 (2013): 2-6
Reduction of Tunnel Enlargement With Use of Autologous Ruptured Tissue in Anterior Cruciate Ligament Reconstruction: A Pilot Clinical Trial
http://www.arthroscopyjournal.org/article/S0749-8063(13)01329-7/abstract
Reducción del túnel de ampliación con el uso de tejido autólogo Ruptura de ligamento cruzado anterior de reconstrucción: un ensayo clínico piloto
Recibido 28 de agosto 2013 ; aceptado el 17 de diciembre de 2013. publicado en línea el 27 de febrero 2014 . Prueba corregida
propósito
Para comparar la ampliación del túnel de doble haz ( DB ) reconstrucción del ligamento cruzado anterior ( ACLR ) con y sin sutura de tejido autólogo a la ruptura de injerto de tendón de la corva en pacientes con anterior subaguda lesión de ligamento cruzado .
Métodos
Diez pacientes con subaguda ( ≤ 3 meses después de la lesión ) ruptura del ligamento cruzado anterior se asignaron aleatoriamente a someterse a DB ACLR con sutura de la ruptura de tejido para injerto de tendón de la corva ( n = 5 ) o convencional DB ACLR ( n = 5 ) . Cuando se utilizó el tejido autólogo de rotura , rotura de tejido remanente se recoge después , dividido en 4 pedazos , colocados entre los bucles en las partes distal y proximal del injerto , que se aseguran con la sutura . A medida que el criterio principal de valoración , la evaluación del volumen de túnel por tomografía computarizada multidetector de 3 dimensiones ( TCMD ) se ha realizado 1 año después de ACLR . Para evaluar la eficacia de estos procedimientos , la puntuación de Lysholm , traducción tibial anterior (medido con un KT- 1000 artrómetro [ MEDmetric , San Diego , CA ] ) , y la inestabilidad rotacional ( medido por la prueba de desplazamiento del pivote ) se evaluaron después de 2 años .
Resultados
La ampliación del volumen del túnel entre 3 semanas y 1 año después de ACLR según la evaluación de la TCMD en 3 dimensiones fue significativamente menor para ACLR usando tejido roto que para ACLR convencional , especialmente en el sitio femoral ( P < 0,05 ) . Sin embargo , la puntuación postoperatoria Lysholm , la estabilidad anterior de la rodilla medida con el KT- 1000 artrómetro , y la tasa de los resultados negativos de las pruebas manuales pivot -shift no difirieron significativamente entre los 2 grupos. No hubo correlación con los resultados clínicos en términos de tamaño del túnel .
Conclusiones
La puntuación de Lysholm , laxitud anterior medida con el KT- 1000 artrómetro , y la inestabilidad de rotación de acuerdo a la prueba de desplazamiento del pivote no difirieron significativamente entre ACLR usando tejido roto y la técnica convencional. Sin embargo , el uso de tejido ACLR ruptura producida la ampliación del túnel femoral menos según la evaluación de la TCMD , que justifica aún más a largo plazo de seguimiento para elucidar su eficacia.
Nivel de evidencia
Nivel II, estudio comparativo prospectivo .
Reduction of Tunnel Enlargement With Use of Autologous Ruptured Tissue in Anterior Cruciate Ligament Reconstruction: A Pilot Clinical Trial
Received 28 August 2013; accepted 17 December 2013. published online 27 February 2014. Corrected Proof
Purpose
To compare the tunnel enlargement of double-bundle (DB) anterior cruciate ligament reconstruction (ACLR) with and without suturing of autologous ruptured tissue to hamstring graft in patients with subacute anterior cruciate ligament injury.
Methods
Ten patients with subacute (≤3 months after injury) anterior cruciate ligament rupture were randomly allocated to undergo DB ACLR with suturing of the ruptured tissue to hamstring graft (n = 5) or conventional DB ACLR (n = 5). When autologous ruptured tissue was used, remnant ruptured tissue was then harvested, divided into 4 pieces, placed between the loops at the distal and proximal portions of the graft, and secured with the suture. As the primary endpoint, tunnel volume assessment by 3-dimensional multi–detector row computed tomography (MDCT) was performed 1 year after ACLR. To assess the efficacy of these procedures, the Lysholm score, anterior tibial translation (measured with a KT-1000 arthrometer [MEDmetric, San Diego, CA]), and rotational instability (measured by the pivot-shift test) were evaluated after 2 years.
Results
Tunnel volume enlargement between 3 weeks and 1 year after ACLR as assessed by 3-dimensional MDCT was significantly less for ACLR using ruptured tissue than for conventional ACLR, especially at the femoral site (P < .05). However, the postoperative Lysholm score, anterior stability of the knee measured with the KT-1000 arthrometer, and rate of negative manual pivot-shift test results did not differ significantly between the 2 groups. There was no correlation to the clinical outcomes in terms of tunnel size.
Conclusions
The Lysholm score, anterior laxity measured with the KT-1000 arthrometer, and rotational instability according to the pivot-shift test did not differ significantly between ACLR using ruptured tissue and the conventional technique. However, ACLR using ruptured tissue produced less femoral tunnel enlargement as assessed by MDCT, warranting further long-term follow-up to elucidate its effectiveness.
Level of Evidence
Level II, prospective comparative study.
Reducción del túnel de ampliación con el uso de tejido autólogo Ruptura de ligamento cruzado anterior de reconstrucción: un ensayo clínico piloto
Recibido 28 de agosto 2013 ; aceptado el 17 de diciembre de 2013. publicado en línea el 27 de febrero 2014 . Prueba corregida
propósito
Para comparar la ampliación del túnel de doble haz ( DB ) reconstrucción del ligamento cruzado anterior ( ACLR ) con y sin sutura de tejido autólogo a la ruptura de injerto de tendón de la corva en pacientes con anterior subaguda lesión de ligamento cruzado .
Métodos
Diez pacientes con subaguda ( ≤ 3 meses después de la lesión ) ruptura del ligamento cruzado anterior se asignaron aleatoriamente a someterse a DB ACLR con sutura de la ruptura de tejido para injerto de tendón de la corva ( n = 5 ) o convencional DB ACLR ( n = 5 ) . Cuando se utilizó el tejido autólogo de rotura , rotura de tejido remanente se recoge después , dividido en 4 pedazos , colocados entre los bucles en las partes distal y proximal del injerto , que se aseguran con la sutura . A medida que el criterio principal de valoración , la evaluación del volumen de túnel por tomografía computarizada multidetector de 3 dimensiones ( TCMD ) se ha realizado 1 año después de ACLR . Para evaluar la eficacia de estos procedimientos , la puntuación de Lysholm , traducción tibial anterior (medido con un KT- 1000 artrómetro [ MEDmetric , San Diego , CA ] ) , y la inestabilidad rotacional ( medido por la prueba de desplazamiento del pivote ) se evaluaron después de 2 años .
Resultados
La ampliación del volumen del túnel entre 3 semanas y 1 año después de ACLR según la evaluación de la TCMD en 3 dimensiones fue significativamente menor para ACLR usando tejido roto que para ACLR convencional , especialmente en el sitio femoral ( P < 0,05 ) . Sin embargo , la puntuación postoperatoria Lysholm , la estabilidad anterior de la rodilla medida con el KT- 1000 artrómetro , y la tasa de los resultados negativos de las pruebas manuales pivot -shift no difirieron significativamente entre los 2 grupos. No hubo correlación con los resultados clínicos en términos de tamaño del túnel .
Conclusiones
La puntuación de Lysholm , laxitud anterior medida con el KT- 1000 artrómetro , y la inestabilidad de rotación de acuerdo a la prueba de desplazamiento del pivote no difirieron significativamente entre ACLR usando tejido roto y la técnica convencional. Sin embargo , el uso de tejido ACLR ruptura producida la ampliación del túnel femoral menos según la evaluación de la TCMD , que justifica aún más a largo plazo de seguimiento para elucidar su eficacia.
Nivel de evidencia
Nivel II, estudio comparativo prospectivo .
jueves, 6 de marzo de 2014
Otra lesión deja a David Pocock fuera de las canchas
http://www.rugbytime.com/noticia.php?id=41384
Otra lesión deja a David Pocock fuera de las canchas
Otra lesión deja a David Pocock fuera de las canchas
El australiano deberá afrontar al menos nueve meses de recuperación al confirmarse una nueva lesión en una de sus rodillas. Es la segunda vez que debe ser operado en apenas de un año
Poca duración tuvieron las ilusiones de Brumbies y David Pocock con respecto a la incipiente participación del experimentado tercera línea en la actual temporada del Súper Rugby.
El jugador estuvo casi un año sin jugar, entre 2013 y principios de 2014, debido a una lesión de ligamentos cruzados y a los 25 años deberá afrontar ahora un nuevo periodo de rehabilitación, el cuál se estima le demandará los próximos nueve meses.
|
miércoles, 5 de marzo de 2014
Ligamento Cruzado Anterior y lesiones ligamentarias de rodilla
http://www.clinicacemtro.com/index.php/es/63-biblioteca/traumatologia-ortopedia-y-medicina-del-deporte/626-ligamento-cruzado-anterior-y-lesiones-ligamentarias-de-rodilla
DEPARTAMENTO DE TRAUMATOLOGÍA. UNIDAD DE RODILLA. CLINICA CEMTRO
La rodilla es una articulación que comprende tres huesos: el fémur, la tibia y la rótula. Esta articulación está estabilizada por unas estructuras dinámicas y estáticas. Entre las estructuras estáticas tenemos los ligamentos de la rodilla:el ligamento lateral interno, el ligamento lateral externo y los ligamentos cruzados: el ligamento cruzado anterior ( el mas conocido por sus implicaciones en el deporte ) y el posterior.
Una lesión del Ligamento Cruzado Anterior (LCA) es un desgarro en el mismo. El LCA se encuentra en el medio de la articulación de la rodilla y conecta la tibia con el fémur. Estabiliza la rodilla al evitar que el fémur pueda desplazarse en exceso hacia adelante causando episodios de inestabilidad en la rodilla.
Las causas de lesión del LCA son múltiples, el LCA es una estructura biológicamente adaptada y mecánicamente bien diseñada para una actividad normal, pero que cuando aumentan la exigencia sobre él, como ocurre en el deporte, o se somete a posiciones inadecuadas, puede romperse con mucha facilidad. La mayoría de las roturas del Ligamento Cruzado Anterior se producen por el apoyo sobre un sólo pie en las caídas- saltos, o por frenar súbitamente en la carrera, aunque las condiciones concretas que influyen en la deformación del LCA no se conocen.
A la hora de realizar un tratamiento en las lesiones del LCA debemos valorar mucho al tipo de paciente que tenemos que tratar, su actividad deportiva, sus requerimientos, y la clínica que presenta el paciente, ya que en muchos casos la intervención quirúrgica no es la mejor opción de tratamiento.
Cuando está indicada la cirugía, la intervención quirúrgica se realiza, generalmente, mediante una técnica artroscópica (introduciendo una microcámara y un instrumental especial a través de pequeñas incisuras en el lateral de la rodilla). En la cirugía sustituimos el ligamento cruzado anteriorafectado por un tendón, que puede ser del propio paciente, y que con el tiempo. biológica y mecánicamente realizará la función del ligamento desgarrado, estabilizando la articulación.
Una vez realizada la reparación del LCA con éxito, el paciente permanece 24 horas ingresado en el centro hospitalario para posteriormente empezar un exhaustivo tratamiento rehabilitador que le permitirá realizar actividades deportivas intensas aproximadamente a los 6 meses.
Respecto al tratamiento de las otras lesiones ligamentarias, cabe destacar que no todas ellas precisan un tratamiento quirúrgico: En el caso del ligamento cruzado posterior, su lesión aislada puede cicatrizar con una buena inmovilización; el ligamento lateral interno rara vez precisa su reparación quirúrgica; y respecto al ligamento lateral externo, por su forma cordonal, cuando se lesiona y se rompe, si precisa reparación quirúrgica.
Un apartado especial serían las lesiones combinadas de ligamentos, como ocurre en las luxaciones de rodilla, situaciones extremadamente delicadas donde hay que valorar y planificar con minuciosidad qué estructuras lesionadas van a precisar reparación quirúrgica, así como tratar todas las posibles lesiones asociadas que puedan ocurrir, tanto intraarticulares como extraarticulares (lesiones neurológicas, vasculares).
lunes, 3 de marzo de 2014
Realizan en España el primer implante de condrocitos autólogos en la cadera
http://traumatologia.diariomedico.com/2013/09/27/area-cientifica/especialidades/traumatologia/realizan-en-espana-el-primer-implante-de-condrocitos-autologos-en-la-cadera
Realizan en España el primer implante de condrocitos autólogos en la cadera
La Clínica Cemtro ha realizado el primer implante de condrocitos autólogos para el tratamiento de cartílago en cadera.
Redacción | 27/09/2013 11:48
Un equipo de clínica Cemtro ha realziado la primerva intervención quirúrgica en la que se ralizó un implante de condrocitos autológos en cadera. Este nuevo avance médico ha desarrollado su trabajo a través de la creación de células en laboratorio que son posteriormente implantadas en la zona a tratar.
El procedimiento para esta intervención consiste, en primer lugar, en extraer mediante artroscopia de cadera una muestra de cartílago de otra zona de la articulación. De esta muestra de cartílago se realiza un cultivo en el laboratorio, en este caso en Laboratorios Amplicel, y tras 4-6 semanas de cultivo se consiguen la cantidad necesaria de condrocitos para realizar el implante. En un segundo tiempo quirúrgico se interviene al paciente en la que se desbrida la lesión del cartílago, se limpian los bordes quirúrgicos y después se coloca una membrana de colágeno recortada a la medida de la lesión, en la que se han instilado los condrocito, y esta membrana se fija al hueso subyacente, mediante sutura ósea, o al cartílago adyacente. Sobre la membrana se pone una capa de Tissucol para sellar los puntos y facilitar el agarre del implante.
Suscribirse a:
Entradas (Atom)





